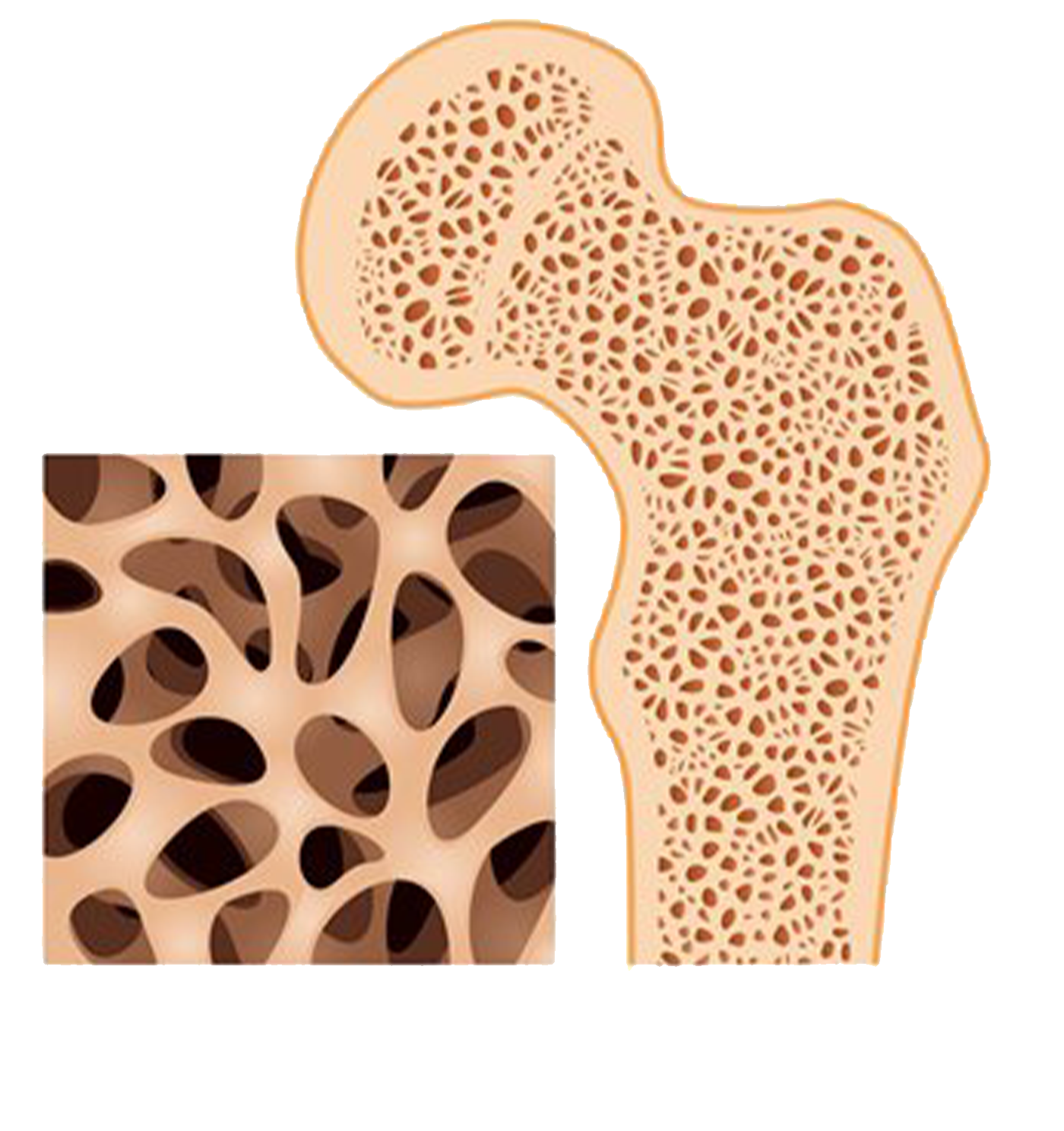
Porous Bone Disease
What is Osteoporosis?
Osteoporosis is a condition of decreased bone mass. This leads to fragile bones that are at an increased risk for fractures. In fact, it will take much less stress on an osteoporotic bone to cause it to fracture than it would on a healthy bone.
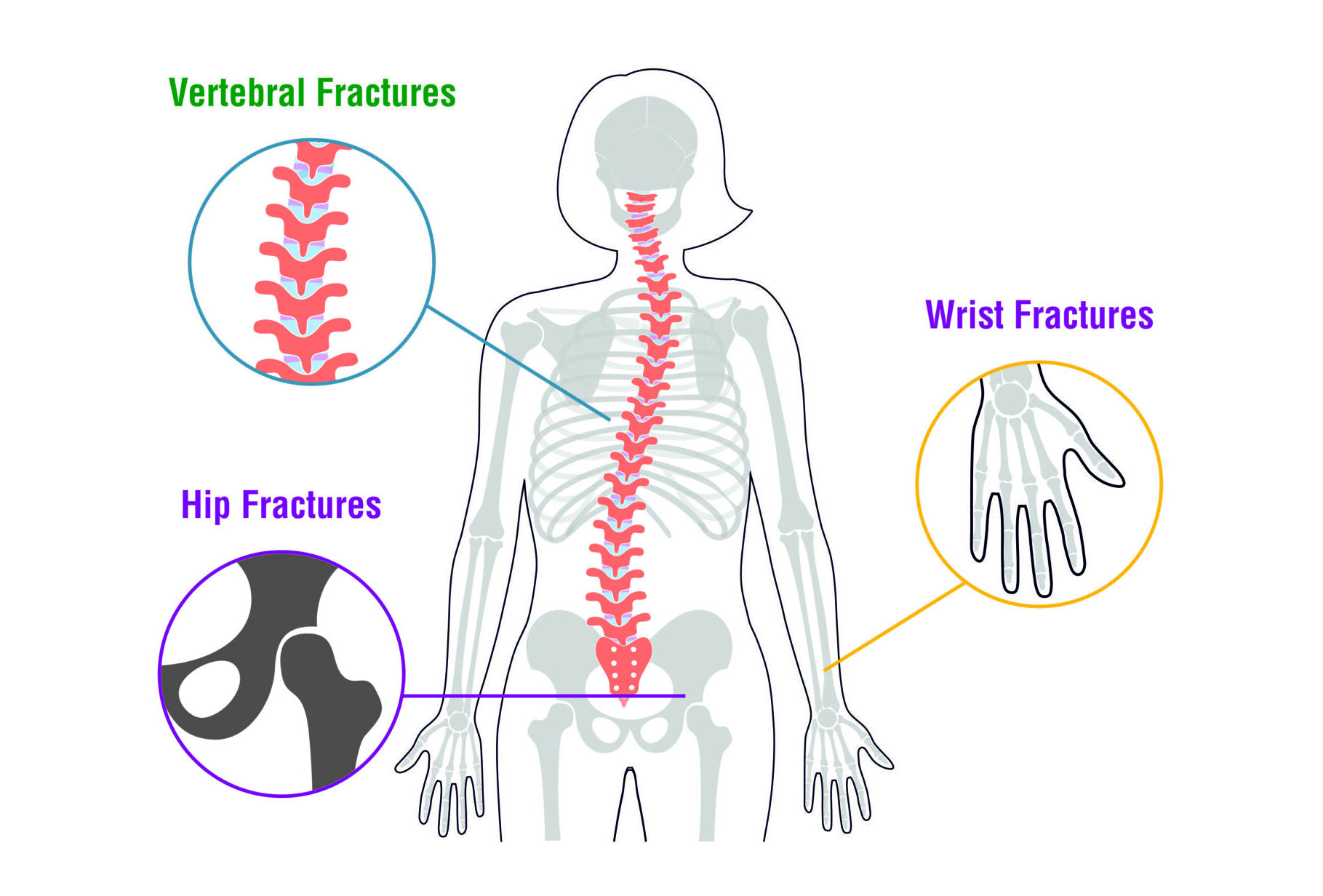
Common fractures which are seen in osteoporotic patients are mostly in the hip, spine, and wrist.
Porous Bone Disease
What is Osteoporosis?
Osteoporosis is a condition of decreased bone mass. This leads to fragile bones that are at an increased risk for fractures. In fact, it will take much less stress on an osteoporotic bone to cause it to fracture than it would on a healthy bone.
Common fractures which are seen in osteoporotic patients are mostly in the hip, spine, and wrist.
What causes Osteoporosis?
to and exacerbate the onset of osteoporosis. They include

Other medical conditions
Such as kidney disease, rheumatoid arthritis, etc.

Reduced sex hormone levels
Estrogen (in women) or testosterone (in men) decline.

Poor diet
Inadequate nutrition affects bone health

Medical conditions that weaken calcium absorption

Corticosteroids & Antiseizure medicines
Medications impacting bone density

Low Testosterone Levels (Men)
Hormonal imbalance affecting bone strength.

Aging
Calcium and Vitamin D deficiency

Thin and/or small frame

Inactive lifestyle
Family history
Smoking
Increases risk of osteoporosis

Alcohol

Women & Post-menopausal women
Higher vulnerability due to hormonal changes
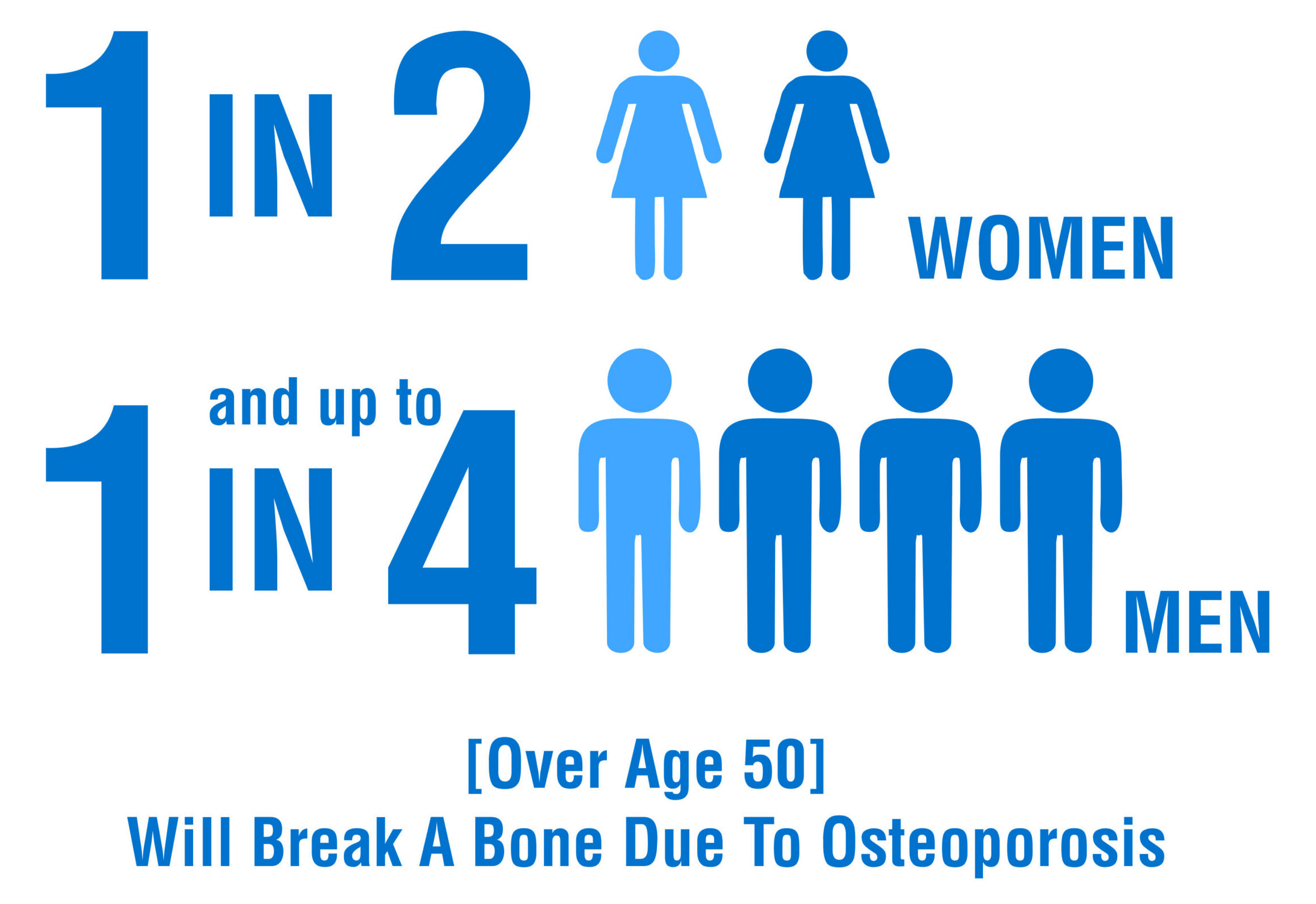
Who is at risk of Osteoporosis?
Some of the most common osteoporosis risk factors include

Female Gender

Family history of osteoporosis


Being Older

History of broken bones


Inactive lifestyle

Smoking

Eating a diet low in calcium and Vitamin D
Symptoms
What are the symptoms of Osteoporosis?
There are usually no specific symptoms that alert you to the presence of osteoporosis early on in its progression.
You may feel a dull pain in your bones or muscles at the onset of the disease. But in most people, fracture is the first event which hints towards the background osteoporosis. These fractures may lead to loss of height, and you may notice yourself hunching forward. Though these finding are seen in very advanced stages of osteoporosis.

Low Energy Fracture

Sudden Back Pain

Joint Pain

Bone Pain

Stooping and Height Loss
Diagnosed & Evaluated
How is osteoporosis diagnosed and evaluated?
To diagnose osteoporosis and assess your risk of fracture and determine your need for treatment, your doctor will most likely order a bone density scan.
Bone Density Scan (DEXA Scan)
- A bone density scan is the primary method used to diagnose osteoporosis and assess fracture risk.
- Dual-energy X-ray absorptiometry (DEXA or DXA) is the most common technique for measuring bone mineral density (BMD).
- This scan measures the amount of X-rays absorbed by tissues and bone, providing a quantitative assessment of bone density.
T Score and Z Score
- The results of the DEXA scan are converted into T scores and Z scores.
- T score compares bone density to that of a healthy young adult of the same sex and ethnicity.
- Z score compares bone density to that of individuals of the same age, sex, and ethnicity.
- T score is primarily used to estimate fracture risk and guide treatment decisions, while Z score helps identify potential underlying causes for low bone density.
Additional Procedures to Assess Fractures
Bone X-ray: Traditional X-rays can detect fractures in the bone, although they are less sensitive to early-stage osteoporosis.
CT Scan of the Spine: A computed tomography (CT) scan provides detailed images of the spine and can detect fractures, especially those in the vertebrae.
MRI of the Spine: Magnetic resonance imaging (MRI) is sensitive in detecting vertebral fractures and can also identify other spinal abnormalities associated with osteoporosis.
By combining the results of bone density scans with other imaging techniques such as X-rays, CT scans, and MRI, healthcare providers can accurately diagnose osteoporosis, assess fracture risk, and determine appropriate treatment strategies for patients.
FRAX tool (Fracture Risk Assessment Tool) is IOF (International osteoporosis foundation) certified tool to assess the fracture risk in individuals above 45 year age important method of finding your risk of fracture without undergoing extensive investigations.
How is osteoporosis treated?
There are multiple ways to treat osteoporosis. Non-surgical methods include
Exercise
- If you have osteoporosis or fragile bones, regular exercise can help keep your bones strong and reduce the risk of a fracture in the future.
- You may worry that being active means you’re more likely to fall and break a bone. But the opposite is true. A regular, properly designed exercise program may actually help prevent falls and fractures. That’s because exercise strengthens bones and muscles and improves balance, coordination, and flexibility. That’s key for people with osteoporosis.
- Before you start a new workout routine, check with your doctor and physical therapist. They can tell you what’s safe for your stage of osteoporosis, your fitness level, and your weight.
- Some activities recommended to build strong bones include –
- Brisk walking and jogging.
- Dancing, step aerobics and stair climbing.
- Weight trailing with free weights or machines.
- Swimming and bicycling.
Physical therapy
Physical therapy doesn’t heal the broken bones but it gives you better odds of a successful recovery.
Calcium and vitamin D
Drugs and Medications
Prescription drug are often necessary for most of the patients which can act by either reducing further bone loss or by increasing new bone formation. Drugs which prevent bone loss include Denosumab, bisphosphonates, calcitonin and hormonal therapies. On the other hand, Teriparatide acts by increasing bone formation.